News
MASLD & Fatty Liver
Move beyond conventional treatments - explore nature's potential for addressing fatty liver.
Dr. Meghan Zech, ND, FABNO
“Understanding the Condition & Pathways to Healing Your Fatty Liver”
Amidst a growing interest in holistic health, Dr. Meghan Zech uniquely blends scientific rigor with a deep passion for herbal medicine in her approach to Non-Alcoholic Fatty Liver Disease (NAFLD). Beyond conventional treatments, she explores nature’s potential for liver support. If you’re drawn to plant-based remedies for any concern (digestion, sleep, mood, hormones), discover how Dr. Zech’s insightful perspective and the gentle power of herbs might offer a complementary path to well-being.
What is MASLD (formerly called NAFLD)?
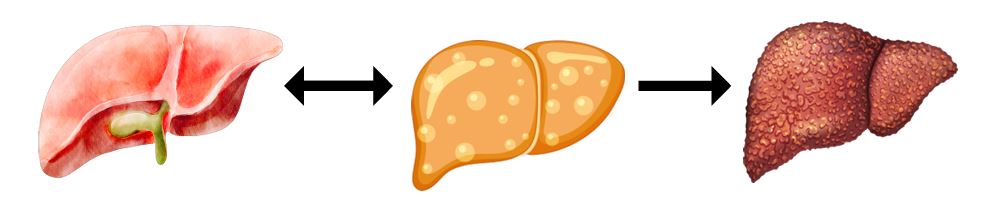
Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD), formerly called Non-Alcoholic Fatty Liver Disease (NAFLD) is a condition characterized by the accumulation of fat in the liver in individuals who do not consume excessive alcohol. MASLD is considered the most common liver disorder in Western countries, affecting an estimated 25-30% of the global population. This condition can be broken down into two main stages: simple fatty liver (steatosis) and the more severe Metabolic Dysfunction Associated Steatohepatitis (MASH). While simple fatty liver may not cause inflammation, MASH involves liver inflammation, which can lead to liver damage and scarring. MASLD is often referred to as a “silent” condition because many individuals experience no symptoms until it progresses. As a result, diagnosis is frequently delayed, allowing the condition to worsen over time.
How MASLD Develops
MASLD develops due to a combination of factors, including poor diet, lack of exercise, metabolic dysfunction, and genetic predisposition. The process often begins with excessive fat storage in liver cells, followed by oxidative stress and chronic inflammation. Over time, these factors lead to scarring and impaired liver function.
The liver plays a critical role in regulating blood sugar, detoxifying the body, and managing metabolism. When the liver is overloaded with fat, its ability to perform these functions is compromised, contributing to a cascade of health issues affecting the entire body
How Sugar and Carbohydrates Contribute to MASLD Progression
Sugar and refined carbohydrates are significant contributors to the development and progression of MASLD. These foods, especially those that are highly processed or contain added sugars, can negatively affect liver function in several ways
1. Insulin Resistance and Fat Accumulation
One of the primary mechanisms by which sugar and refined carbohydrates contribute to MASLD is through the development of insulin resistance. Insulin is a hormone that helps regulate blood sugar levels by signaling cells to absorb glucose from the bloodstream. However, when the body is consistently exposed to high amounts of sugar, the cells become less responsive to insulin. This results in insulin resistance, which is a hallmark of MASLD. As insulin resistance worsens, the liver is forced to work harder to process glucose, leading to an increased storage of fat in liver cells. This excess fat buildup, known as hepatic steatosis, is the first stage of MASLD and is one of the key contributors to liver inflammation. In the long term, this process can lead to MASH (Metabolic DysfunctionAssociated Steatohepatitis, fibrosis and cirrhosis.
2. Excess Fructose and Fatty Liver
Another contributing factor to MASLD progression is the excessive consumption of fructose, a type of sugar found in many processed foods and sugary beverages. Unlike glucose, which is metabolized by all cells in the body, fructose is primarily processed in the liver. When consumed in large quantities, fructose overwhelms the liver’s capacity to metabolize it effectively. As a result, the liver begins to convert excess fructose into fat, leading to fatty liver. Over time, this process can lead to inflammation and scarring. High-fructose corn syrup (HFCS), a common sweetener in sodas, candies and processed snacks, is particularly problematic because it is composed of a high proportion of fructose. Studies have shown that diets high in fructose can promote liver fat accumulation, inflammation, and insulin resistance, all of which exacerbate MASLD.
3. Dysregulated Lipid Metabolism
A diet high in refined carbohydrates (such as white bread, pasta, pastries and sugary cereals) causes rapid spikes in blood sugar levels, followed by insulin surges. These fluctuations can disturb lipid metabolism in the liver. When the liver processes large amounts of sugar and refined carbs, it can lead to an overproduction of triglycerides—a type of fat that accumulates in liver cells and contributes to MASLD. The liver’s inability to manage fat storage efficiently can result in fatty liver disease, which, when left untreated, may progress to more severe stages like MASH. This imbalance in lipid metabolism also increases the risk of cardiovascular disease, as the excess triglycerides can spill into the bloodstream and contribute to plaque buildup in arteries.
4. Chronic Inflammation and Oxidative Stress
Consuming high amounts of sugar and refined carbohydrates not only contributes to fat accumulation but also induces chronic inflammation in the liver. Both glucose and fructose can trigger oxidative stress, which occurs when the body’s antioxidant defenses are overwhelmed by free radicals. This leads to liver cell damage, inflammation and the activation of pathways that promote fibrosis (scarring). Chronic inflammation can worsen liver function, impair detoxification processes, and contribute to a vicious cycle that makes it harder to reverse MASLD. Moreover, high sugar intake is also associated with increased levels of advanced glycation end products (AGEs), compounds that further promote oxidative stress and liver damage.
Long-Term Implications of MASLD
If left untreated, MASLD can progress to MASH, which increases the risk of liver cirrhosis and liver cancer. However, even simple fatty liver can contribute to other serious health conditions, such as:
Cardiovascular Disease: People with MASLD have a higher risk of heart disease, including heart attack and stroke.
Type 2 Diabetes: MASLD can worsen insulin resistance and contribute to the development of type 2 diabetes.
Chronic Kidney Disease: Kidney function may be impaired in those with MASLD due to the systemic metabolic dysfunction.
Increased Cancer Risk: MASH, in particular, is associated with a higher risk of liver cancer (hepatocellular carcinoma), as well as an increased risk of other cancers, including colorectal and pancreatic cancers.
MASH: A Progressive Stage of MASLD
MASH represents a more severe form of MASLD, where fat buildup in the liver causes inflammation and liver cell damage. As MASH progresses, it can lead to liver fibrosis and eventually cirrhosis. Unlike simple fatty liver, MASH can lead to significant health complications and is now the leading cause of liver transplants in the U.S., surpassing hepatitis C.
How MASLD and MASH Can Be Managed
The good news is that both MASLD and MASH are highly treatable conditions, and early intervention can often reverse liver damage, especially when lifestyle changes are made early on.
Nutrition: Support Liver Health Through Food
A liver-friendly diet is crucial for managing and even reversing MASLD. Key dietary principles include: Increase Fiber Intake: Whole grains, vegetables and legumes help stabilize blood sugar and reduce liver fat accumulation.
Healthy Fats: Omega-3 fatty acids (found in foods like salmon, flaxseeds and walnuts) reduce liver inflammation and support metabolic health.
Cut Back on Sugar and Refined Carbohydrates: Reducing intake of added sugars and limiting processed foods is essential for improving liver health.
Antioxidant-Rich Foods: Incorporating antioxidant-rich foods such as berries, leafy greens and nuts can help fight oxidative stress in the liver and support detoxification.

Exercise: Supporting Liver Function
Physical activity is an important component of MASLD treatment. Regular aerobic exercise (such as walking, swimming or cycling) and resistance training (including weight lifting or body weight exercise such as yoga or pilates) both contribute to reducing liver fat, improving insulin sensitivity and lowering inflammation. Aiming for at least 150 minutes of moderate-intensity exercise per week is recommended for optimal liver health.
Emsculpt: A Treatment Option to Support Liver Health
Emsculpt, a non-invasive body contouring treatment available at Village Medicine, can support MASLD management by improving muscle mass and metabolic function. Through radiofrequency heating, Emsculpt helps break down fat cells and stimulate muscle contractions, promoting fat reduction and improved body composition. This can aid in weight management, which is critical for reversing fatty liver disease.
Herbal Medicine for Liver Support
Herbal medicine offers an array of options for supporting liver health, especially through the use of plants that promote detoxification, reduce inflammation and enhance liver function. Many of these herbs are not only medicinal but can also be easily found and foraged in the Pacific Northwest during the spring season.
Foraged Liver-Supportive Herbs:
Dandelion (Taraxacum officinale): Dandelion is a powerful liver tonic and is commonly found in the wild. The leaves help stimulate bile production, which is essential for fat digestion and the detoxification process. Dandelion root can also be used to support the liver’s detox functions. In the spring, young dandelion leaves can be added to salads or made into a refreshing tea.
Nettle (Urtica dioica): Nettle is another herb that is commonly foraged in the Pacific Northwest, especially in the spring. It helps support kidney and liver health by stimulating the elimination of waste products and toxins. Nettle leaves are rich in minerals, including magnesium and iron, which further help detoxify the body. Nettle can be added to soups, stews or teas.
Peppermint (Mentha piperita): While not a wild forage, peppermint is a wonderful herb for supporting digestion and soothing liver inflammation. It also aids in bile flow, which is crucial for liver health and digestion. Fresh peppermint leaves can be easily grown or bought and added to a variety of dishes or teas.
Oregon Grape Root (Mahonia aquifolium): Native to the Pacific Northwest, Oregon grape root has been traditionally used to support liver health. It acts as a natural bile stimulant, helping to detoxify the liver and gallbladder, which is especially beneficial for individuals with fatty liver disease (NAFLD). Oregon grape root also has antimicrobial properties, which can support gut health—another important aspect of liver function. Additionally, the yellow flowers of the Oregon grape are edible and can be added to salads or blended into dressings for a vibrant and health-boosting garnish!
Liver-Supportive Culinary Herbs:
Several common culinary herbs can also support liver health. Cook freely with these herbs both to flavor dishes and support liver function. Let food be your medicine!
Turmeric: Known for its anti-inflammatory properties, turmeric contains curcumin, which helps reduce liver inflammation and promotes detoxification. It is easily incorporated into a wide range of dishes, from curries to smoothies.
Ginger: Ginger is another anti-inflammatory herb that can support digestive function and help with liver detox. It stimulates bile production and is also beneficial for reducing nausea, which is common in those with liver conditions.
Garlic: Garlic contains sulfur compounds that activate liver enzymes, which are essential for detoxification. It also helps reduce oxidative stress and inflammation in the liver.
Lemon: Though technically a fruit, lemon is often used as a culinary herb in various recipes. It helps stimulate bile production and is an excellent source of vitamin C, which supports detoxification and reduces liver inflammation.
Taking Control of Liver Health
MASLD is a common but treatable condition. With early intervention, lifestyle changes such as a healthy diet, regular exercise, herbal support, and cutting-edge treatments like Emsculpt, individuals can reverse liver fat accumulation and improve liver function. The key is recognizing the condition early and committing to long-term, sustainable lifestyle changes.
Liver-Supportive Herbal Tea Recipe
A simple and effective way to support liver health is through a nourishing herbal tea made from liver-friendly plants. Here’s a recipe you can try at home to help cleanse and support your liver:
Spring Liver Detox Tea Ingredients:
- 1 tbsp Dandelion leaf (fresh or dried)

- 1 tbsp Nettle leaf (fresh or dried)
- 1 tsp Peppermint leaves (fresh or dried)
- 1-2 slices fresh Lemon
- 1 tsp fresh Ginger (or 1/2 tsp dried ginger) Honey or stevia to taste (optional)
Spring Liver Detox Tea Instructions:
- Bring 4 cups of water to a boil in a saucepan.
- Once the water is boiling, add the dandelion, nettle and peppermint leaves.
- Reduce the heat and let the herbs steep for 5-10 minutes, depending on how strong you want the flavor.
- Add the fresh ginger and allow it to steep for another 3-5 minutes.
- Remove from heat and strain the herbs out.
- Add a slice of fresh lemon to each cup and, if desired, sweeten with honey or stevia.
- Serve warm or allow it to cool and enjoy it as an iced tea!
* This post was originally printed in the Village Medicine Seattle’s Wellness Quarterly Magazine, 4Q23 Edition. Read and download the full publication

About The Author
Dr. Meghan Zech is a Naturopathic Physician and Fellow of the American Board of Naturopathic Oncology (FABNO) serving patients at Village Medicine Seattle. Meghan believes in an individualized approach to educate and empower patients in order to establish and support sustainable health and well-being.
Learn more about Dr. Zech
